Cavus Foot A foot deformity causing painful and unstable walking, treatable with specific footwear or surgical intervention.
WHAT IT IS
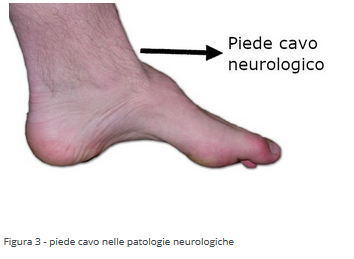
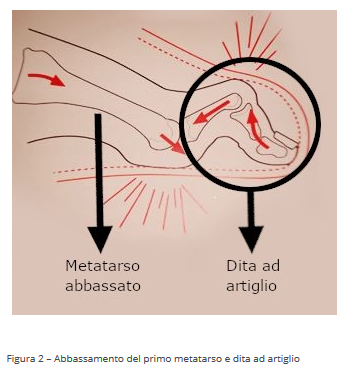
Cavus foot is a deformity that can be congenital or develop after birth. It is characterized by an accentuation of the arch of the foot (Figure 1), varus of the back part of the foot (the heel turns inward), and lowering of the first metatarsal with claw toes (Figure 2).
Cavus foot becomes a true malformation when the arch accentuation becomes excessive (cavism). Deformities of the back (retropiede) and front part (avampiede) of the foot can be associated with cavism, causing the patient to walk, leaning on the outer edge of the foot. In all types of cavus feet, there is retraction of the plantar fascia, a band of muscles and tendons that cover the sole of the foot. The plantar fascia becomes an arch cord, deforming the front part of the foot and the heel. Consequences include:
- Pain when standing or walking
- Difficulty fitting shoes
- Instability of the foot, prone to sprains
CAUSES
Cavus foot is classified into various forms based on the underlying reasons:
Congenital Forms:
- Idiopathic cavus foot (of unknown cause)
- Sequelae of clubfoot
- Multiple joint contractures (arthrogryposis)
Neuromuscular Forms:
- Muscular diseases (myopathies)
- Peripheral nerve disorders like Charcot-Marie-Tooth disease
- Injuries to spinal nerve roots
- Formation of fluid-filled cysts in the spinal cord (syringomyelia)
- Spina bifida
- Spinal muscular atrophy
- Spinal cord neoplasms
- Friedreich's ataxia
- Cerebral palsy
Post-Traumatic Forms:
- Crush injuries to the lower limbs
- Severe burns
- Sequelae of severe muscle or bone damage causing reduced blood flow to the affected limb (ischemia)
- Post-traumatic arthritis
In neurological conditions, cavus foot (Figure 3) results from muscle imbalance. In polio, a particularly severe form of cavus foot can develop.
SYMPTOMS
Symptoms reported by children and parents vary, with the most frequent being:
- Pain when the child stands or walks
- Pain and ulceration of the toes
- Reduced joint mobility limiting the foot's ability to absorb impact
- Easy fatigue during walking
- Calluses on the sole of the foot and toe tips
- Repeated ankle sprains
DIAGNOSIS
Diagnosis involves a thorough collection of the child's history and a similarly meticulous examination. The primary examination is weight-bearing foot and ankle X-rays (with the patient in an upright position), revealing varus of the heel, abnormal flexion of the metatarsal, and possible arthritis. Magnetic Resonance Imaging (MRI) can highlight ligament and cartilage damage from repeated ankle sprains.
TREATMENT
Conservative Therapy:
The goal is to ensure balanced weight distribution on the sole of the foot. This can be achieved using corrective semi-flexible footwear (orthoses) or custom-made footwear with possible leg and foot braces, especially useful in neurological diseases.
Surgical Therapy:
The aim of surgical treatment is to achieve balanced support on the sole of the foot and provide walking stability. If the foot is flexible, the plantar fascia is severed, taking a portion of the tendon from a functioning muscle and inserting it where a non-functioning muscle is. If the foot is rigid, osteotomies and arthrodesis are performed, meaning surgical fractures of the foot bones that are repositioned and reattached with plates and screws. To correct claw toes, tendon transfers are performed by taking a portion of the tendon from a functioning muscle and inserting it where a non-functioning muscle is. Additionally, the so-called "hallux arthrodesis" can be performed, aligning and fusing two bones of the big toe to eliminate deformity. Corrective cuts (osteotomies) are made for the heel. After bone procedures, the patient is protected with a plaster leg brace, which is removed after a month. Physiotherapy is conducted after plaster removal.
PROGNOSIS
Prognosis is better for idiopathic forms. The prognosis is less favorable for neurological forms influenced by the underlying disease.e.
written by: Rosa Russo, Pier Francesco Costici - Orthopedics Operational Unit In collaboration with Bambino Gesù Institute for Health original article
from: ospedalebambinogesù.it