Infantile cerebral palsy: foot deformities
Foot deformities in cerebral palsy arise from muscle imbalances and subsequent motor coordination disorders, with the most common being equinus and clubfoot.
Causes of Foot Deformities:
Muscle imbalance between agonist and antagonist muscles, intensified by spasticity affecting certain muscles more than their opposing counterparts, and coordination disorders causing uneven joint stress, can result in incorrect foot placement. This, in turn, can lead to malfunctioning leg joints such as the knee and hip.
Common Foot Deformities:
The most frequent foot deformities include:
- Equinus Foot
- Clubfoot
- Valgus Pronated Flat Foot
EQUINE FOOT
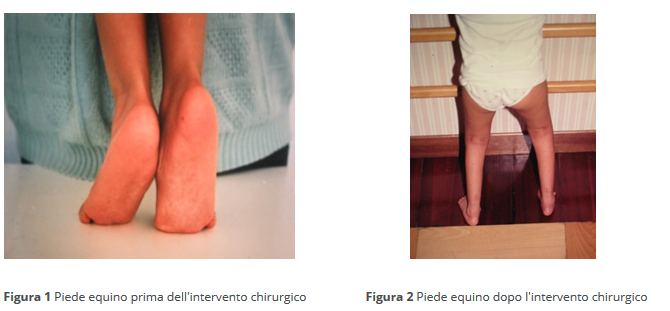
Equinus foot is characterized by toe-walking (Figure 1). This deformity results from the dominance of plantar flexor muscles (agonist muscles) due to abnormal muscle tone (neurological hypertonicity). The Achilles tendon shortens, preventing the rear part of the foot (heel) from making contact with the ground. Patients walk on their toes, reducing the base of support and causing compensatory flexion of the knees and hips. Treatment varies with the patient's age and the reducibility of the deformity, i.e., the ability to manually bring the joint back to its normal position.
If equinus is manually correctable (reducible), involving bringing the foot beyond 90°, the treatment is conservative. It includes rehabilitation aided by orthopedic corrective devices (orthoses) and local injections of botulinum toxin. Abnormal plantar flexion causing equinus is a result of triceps surae muscle spasticity. Local botulinum toxin injection relaxes the muscle, alleviating equinus symptoms.
If equinus is not manually reducible, the treatment becomes surgical, often involving percutaneous Achilles tendon lengthening with a micro scalpel (fibrotomy - Figure 2). Conservative approaches are typically preferred for younger children unless the deformity is severe and only surgically correctable.
Minimally invasive surgical Achilles lengthening can be repeated during the growth phase.
CLUBFOOT
Clubfoot (equinus, varus, supinated) is characterized by resting on the lateral edge and tip of the foot (Figure 3). The heel appears elevated due to Achilles tendon retraction and rotated inward. The posterior tibial tendon prevails over antagonist muscles, pulling the foot inward and onto the lateral edge. Treatment principles for clubfoot align with those for equinus. If the deformity is reducible, treatment involves rehabilitation, orthoses, and botulinum toxin.
If the deformity is not manually reducible, decisions regarding age and reducibility determine whether to perform soft tissue interventions (tendons, capsules, muscle fascia) or bony interventions. For younger age groups, Achilles tendon and posterior tibial tendon lengthening are commonly performed (Figure 4). In individuals over 13 years old, if the deformity is rigid (not reducible), osteotomy and arthrodesis procedures are done, surgically repositioning and synthesizing foot bones using means like screws, plates, and wires (Figures 5 and 6).
VALGUS PRONATED FLAT FOOT
Characterized by resting on the inner edge of the foot, valgus pronated flat foot is linked to a predominance of pronation force over supination. Pronation involves the inward movement of the foot, while supination involves the opposite. Clinically, the foot appears flat, with the front part (forefoot) pronated, the heel valgus (deviated outward), and often raised due to associated Achilles tendon retraction. Treatment follows the same principles as other described deformities, with conservative measures such as rehabilitation and orthoses (insoles, footwear, braces) for early stages.
In cases where the non-reducible valgus pronated flat foot is less severe, surgical intervention involves applying a screw (arthrodesis procedure) to prevent excessive pronation and elevate the arch (Figures 7, 8, 9, 10). For more severe forms in individuals older than thirteen, osteotomy and arthrodesis surgeries are performed (Figures 11, 12, 13, 14).
written by: Pier Francesco Costici, Rosa Russo, Fabrizio Donati - Orthopedics Operational Unit in collaboration with: Bambino Gesù Institute for Health
original article from: ospedalebambinogesù.it